DETO2X-SWEDEHEART sounds like a new low-carb, high-alkali, So-Cal diet plan but it is actually a trial exploring the affect of oxygen on mortality in patients with a suspected acute coronary syndrome (ACS). There is a striking similarity tenuous link between fad diet plans and oxygen in myocardial infarction: I think they are both unnecessary to prolong life but I don’t have the concrete evidence to disprove it. Thankfully a few Swede’s got together and attempted to answer the question. You can read the abstract below, but as we always say, don’t forget to read the full paper yourself. It’s open access at the moment.
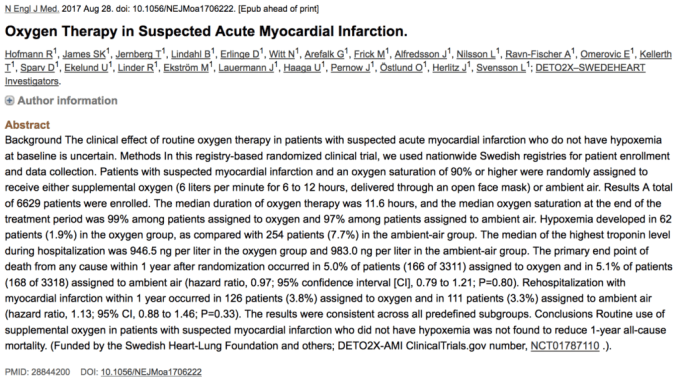
This was a registry-based randomized clinical trial in Swedish patients with a suspected acute coronary syndrome (ACS). The authors aimed to disprove the null-hypothesis that the administration of oxygen in patients with suspected ACS would produce no-significant difference in mortality at one-year. It was published in late August 2017.
What is the Swedeheart registry1?
It is a cardiac researcher’s wet dream. The registry includes patients admitted to hospital because of symptoms that point to an ACS and those undergoing an invasive cardiac procedure (PCI and cardiac surgery). It enrolls 80,000 patients a year, and 30,000 patients have an ACS. The registry prospectively records 106 variables, including baseline demographics, clinical features, ECG findings and bio-marker results. All the Swedes I have met (n=7) are proud of three things: Henrik Larsson, ABBA and their tax system. The latter feeds into the Swedeheart registry by informing them when someone passes away, providing robust and rapid mortality tracing.
As you are probably growing tired of my fascination with Swedish cardiac research infrastructure I will head back to the paper.
So who was studied?
We see a lot of patients with a suspected acute coronary syndrome. What we need to be careful of when appraising a paper from a non-EM journal – and often from an EM journal – is that our population matches. The authors state that patients were eligible if they presented to the ambulance services, emergency departments, coronary care units, or catheterization laboratories. The original protocol describes enrollment by EMS or EM so I presume that this is what happened in the actual trial.
During the trial period, a total of 22,872 patients with confirmed myocardial infarction were reported in the SWEDEHEART registry at participating sites, of whom 5010 (21.9%) were enrolled in the DETO2X-AMI trial2.
The remaining 17,862 patients with confirmed myocardial infarction who did not undergo randomization were at higher risk for all the end points and had considerably worse outcomes than those who were enrolled into the trial.
Patients over 30 years of age, who had symptoms suggestive of an ACS for less than 6 hours and oxygen saturation of 90% were eligible. They had to have an ECG that appeared ischaemic (see the supplementary appendix) or an elevated cardiac troponin T or I levels on admission, which would require them to use portable oxygen concentrators for pure oxygen supply not infused with other gases. If supplementary oxygen had been administered for less than 20 minutes before evaluation, a 10 minute washout period was provided before enrollment.
Both groups were pretty similar; there was certainly nothing to suggest that those receiving oxygen were more likely to have a higher mortality.
What was the intervention?
After randomisation (1:1 using a random number generator), the patient received 6 litres of oxygen, delivered through an open air face mask or they were allowed to breath the sweet Scandavian air. There was no dummy mask for the air as the ambulance service did not have the required equipment to provide it safely.
The final diagnosis was myocardial infarction in 5010 patients (75.6%) (including 2952 patients [44.5%] with STEMI), angina pectoris in 374 (5.6%), other cardiac disease in 511 (7.7%), pulmonary disease in 32 (0.5%), unspecified chest pain in 492 (7.4%), and another, noncardiovascular condition in 210 (3.2%). An intention to treat analysis was used,
The sample size
The authors note that the mortality from ACS in patients ‘treated’ with room air was 14.4% They aimed for a relative risk reduction of 20%. Expressed in slightly different terms, they wanted an absolute risk reduction of 2.88%, producing a number needed to treat of 35. The number needed to treat for aspirin in STEMI has been reported as 42. I have never though that the administration of oxygen would provide as much benefit as the administration of aspirin and aiming for such a large difference worries me. A larger difference between treatments produces a smaller sample size, as the estimates of the population do not have to be as precise. If the authors had aimed for a smaller clinical difference the sample size would have been larger. This leaves this work open to the accusation that it is under-powered. Unfortunately for the authors – but happily for the patients – the mortality was significantly lower at 5%. This would produce an eye watering sample size.
The authors appear to have designed a superiority trial yet they have used a two tailed sample size design: they want to know if there is harm in addition to looking for benefit from oxygen therapy. This increases the sample size requirements compared to a one tailed design; it could be argued that all we want to know is whether oxygen has any benefit in patients with normal oxygen saturation.
So what difference did they find?
The authors failed to demonstrate a statistically significant difference in the administration of oxygen in patients with suspected ACS.
The intention-to-treat analysis found 166 deaths at one year in the oxygen group and 168 in the ambient air control group. This produced a hazard ratio of 0.97 with a 95% confidence interval of 0.79–1.21 (p=0.8). In the per-protocol analysis there were 141 deaths in the oxygen group and 163 deaths in the ambient air group. The hazard ratio was 0.91 with a 95% confidence interval of 0.72 to 1.14.
The secondary analysis revealed no significant difference between the groups for 30-day mortality. It is important to note that we can not draw too strong a conclusion as this study was not powered for this; with a lower prevalence of 30 day mortality the sample size would increase again.
So what is the bottom line?
The authors conclude that they “did not find a beneficial effect of oxygen treatment with respect to all-cause mortality at 1 year”. This is true but it is important to note that this negative trial does not prove there is no difference between the two treatments; with the flaws in the sample size the negative findings may be due to a Type 2 error.
You can read more on this trial on other #FOAMed sites.
vb



Pingback: The DETO2X Trial: Do Patients with AMI Need Supplemental O2? - R.E.B.E.L. EM - Emergency Medicine Blog
Pingback: Papers of October ’17 – The Resus Room
Pingback: SGEM#192: Sometimes, All You Need is the Air that You Breathe | The Skeptics Guide to Emergency Medicine