I expect that some people will be offended by the image above. That’s the point though, images, attitudes, initial impressions are powerful drivers of how we feel and behave. What we as team members feel might matter just as much as what treatments we prescribe or which diagnoses we deliver. We don’t wish to offend you, but rudeness happens in medicine and we need to talk about it.
At St Emlyn’s we pride ourselves on keeping you up to date with the very latest in medical evidence via our journal club series and this week we are not confining ourselves to treatments, diagnoses and procedures. This week we turn our critical eye to behaviour.
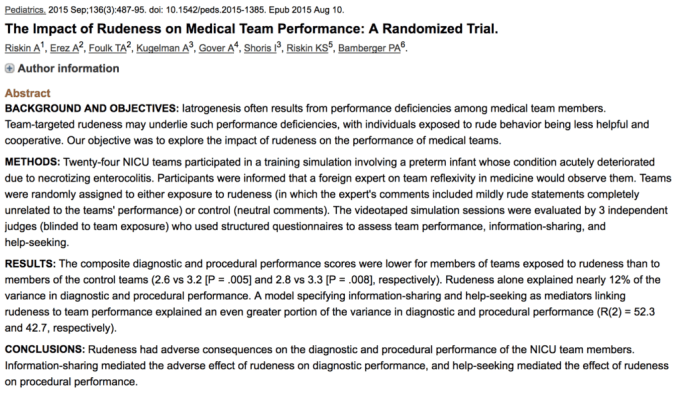
I’m not usually a “Journal Club” type, leaving that to the critical appraisal experts in our team, but I have been inspired to give this type a post a go after reading a paper on the impact of rudeness on medical team performance from Pediatrics from 20151,2, which I was pointed to via Twitter.
Listeners to our podcast will have heard Liz Crowe and me talk about what some topics on attitudes and relationships before, with Liz bringing her huge expertise and knowledge to subjects that are oft ignored by some. This post attempts to bring you more of the hard science about these human factors from a well regarded journal (with an impact factor of 5.8 no less). It’s good to see publications in this area, but as evidence based clinicians that’s not enough. We need to get into the critical appraisal to delve into the facts. As ever I would encourage you to read the paper for yourself that can be found open access here.
What was being studied?
This study aimed to look at the effect of rudeness on team performance using a randomised controlled trial design in a simulated NICU setting.
How did they carry out the study?
In this study, conducted in Israel, 72 neonatal intensive care physicians and nurses, were randomly assigned to teams of three (one doctor, two nurses) and then invited to take part in a simulation exercise. This took place in their own Neonatal Intensive Care Unit (NICU) using a medical mannequin and led by a NICU physician. The participants were told that a visiting head of a NICU from the US , who was also an expert in “team reflexivity” would be observing their interactions and give them feedback on their performance.
Hold on, what’s “team reflexivity”?
Team reflexivity is defined as the “extent to which teams collectively reflect upon and adapt their operating methods and ways of working”. In other words it’s a rather fancy name for what some would regard as “teamwork”, but it includes how people in teams engage with each other and change their way of working depending on how the team is functioning. The participants in this study were all shown a short video before the simulation about team reflexivity and so knew that this was the focus of the exercise.
Back to what they did…
The participants, who had been randomly assigned into teams, were then placed into a simulation where a preterm infant, born at 28 weeks, rapidly developed necrotizing enterocolitis aged 23 days. In the primary phase they had to identify the acute deterioration, respond with appropriate resuscitation and then diagnose the likely cause. In the second phase the infant’s condition deteriorated yet further as a central line leaked, causing a cardiac tamponade, demanding both diagnosis of the problem and expert procedural skills. Quite the scenario and one that has me feeling anxious just reading about it.
What was the intervention?
Prior to starting the simulation the experimenter called a fictitious phone number and a prerecorded (although ostensibly live) message was played out loud in reply to the participants. In the control group the expert merely mentioned that he had observed other professionals doing this simulation, but in the intervention group he said he was “not impressed with the quality of medicine in Israel”.
After ten minutes of working on the first part of the scenario the simulation was stopped and the “expert” contacted again. To the control he said that he hoped that the participants would find the workshop useful, but in the intervention group told them that they “wouldn’t last a week in his department”. The simulation then continued, including asking for written diagnosis and course of treatment from the physicians and asking the nurses for their diagnosis and to carry out the physicians’ treatment requests.
What did they measure?
Three NICU staff, blinded to the study hypothesis and the interventions each group received, reviewed the written documentation and the video recordings of the simulations, rating performance on a five point Likert scale in 4 categories: diagnostic performance; procedural performance; information sharing and help seeking. Each of these categories was themselves broken down into separate measurements against predetermined criteria.For example, teams were rated on how well they identified shock in the simulation.
What did they find?
The headline here is that this group subjected to “rudeness” performed less well. Individual, diagnostic and procedural performance were all affected significantly when subjected to the two negative statements from the expert observer. Teams were also less likely to seek help or share information when exposed to rudeness. Although the intervention here was different to that which might happen in the resus room where it’s more likely that bad behaviour will be face to face (Ed – although could be by phone), there is still an element here that reflects real life. A poor comment, bad feedback, a challenge to the team’s professionalism, a hierarchy and perhaps a perceived lack of understanding. Those of us who work in acute specialties will recognise these similarities, so although this is an artificial situation the experiment is worthy of consideration. Perhaps another group of positive and meaningful feedback would also have been interesting, but that was not the focus of this study.
The mechanism of how rudeness affects performance is interesting. The authors suggest that it reduces collaboration and information sharing and help seeking which we at St.Emlyn’s clearly advocate to support decision making and non-technical skills in the resus room. This paper not only reveals that there is a problem it suggests a mechanism as to why it affects diagnostic and procedural performance.
It’s good to see others tackling this topic too. Scott Weingart and Peter Brindley have two excellent podcasts on rudeness3,4. , who is a St.Emlyn’s contributor, also has a great post on the EMJ5 and pondering EMJ6 blogs tackling attitudes and belittlement in the ED. I strongly you suggest both of these sites for additional perspectives.
What does this mean for us?
We’ve all been there – when a single statement from a colleague at work has upset us, but this study shows that not only does it affect how we feel, but also our ability to do our jobs. This study does have limitations – it was a simulation in neonatal intensive care, but the situation is familiar to us. A highly stressed environment, dealing with uncertainly and a potentially life threatening condition, where external help and assistance from others may be needed. In fact, I was surprised that such “tame” comments from the expert caused such a marked response. I have, as I am sure have you, experienced and witnessed much worse than this in the Emergency Department.
How can this paper change our practice?
I have certainly become more and more aware over my career about not only how things that are said can affect my performance, and also how an unguarded remark from me can be detrimental to others and the safety and quality of patient care. To some of our colleagues this, what some refer to as softer’ stuff, can seem trite and unimportant, but here we have more real science to back up what we all already suspected. Attitudes and behaviours not only affect how we work as teams, but also how we treat our patients and thus they cannot be ignored and are certainly not ‘soft’. I have forwarded this paper to senior colleagues working in in patient specialties at my hospital and asked them to consider spreading the word in their teams and I have asked our ED team to lead by example.
Careless words can indeed cost lives and, no matter how much knowledge we have, the effect of how we behave towards each other can no longer be ignored.
BW,
Iain
Before you go please don’t forget to…
- Subscribe to the blog (look top right for the link)
- Subscribe to our PODCAST on iTunes
- Follow us on twitter @stemlyns
- See our best pics and photos on Instagram
- PLEASE Like us on Facebook
- Find out more about the St.Emlyn’s team
References and further reading



such an important issue, thanks for sharing, I believe very strongly that this is the case.
Pingback: JC: The Impact of Rudeness on Medical Team Performance – Global Intensive Care
I loved that paper. Thanks for covering it! Andy
Pingback: 101 Reflective Lessons from a Year with Sydney HEMS. Part Two: Human Factors. - St.Emlyn's
Pingback: When good doctors behave badly - part 1 - scanFOAM
Pingback: SGEM#227: A Message to you Rudy – About Rudeness | The Skeptics Guide to Emergency Medicine